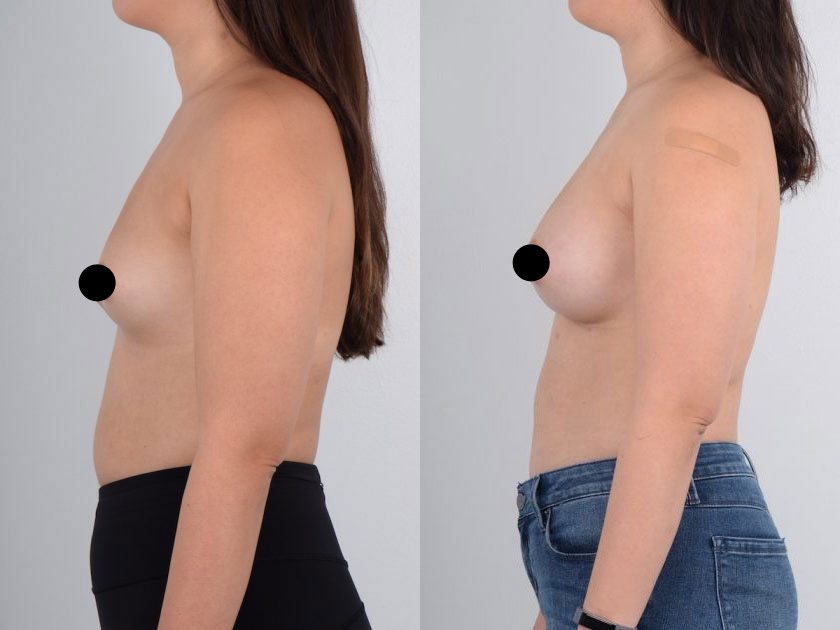
Breast Augmentation
 The approach used in Breast Augmentation is determined by a patient’s individual needs. Before surgery, the type of approach that should be used is determined during consultation. The two that are recommended by Dr. Kim for Asians interested in Breast Augmentation are Inferior breast crease/inframmary fold (IMF) and axillary/transaxillary, but others are listed for consideration.
The approach used in Breast Augmentation is determined by a patient’s individual needs. Before surgery, the type of approach that should be used is determined during consultation. The two that are recommended by Dr. Kim for Asians interested in Breast Augmentation are Inferior breast crease/inframmary fold (IMF) and axillary/transaxillary, but others are listed for consideration.
Incision Techniques
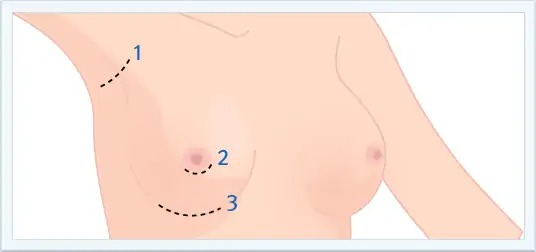
AXILLARY/TRANSAXILLARY
#1) This incision is made at the axillary crease. The resulting scar will fade over time, is not highly noticeable, and is not a significant concern for women who wear sleeveless clothing. The scar in this area tends to heal well but it can create visible scar in patients who are prone to scarring. In that case, scar revision can be performed. The disadvantage of this incision is that it requires specialized skill to meticulously dissect without damaging the chest muscle and creating pain. Furthermore, in order to prevent any bleeding, the use of an endoscope is needed. The endoscope allows a clear visualization of the surgical area and assists in precise dissection.
This procedure is ideal for patients for whom visible scars on the breasts are not desirable such as those who are in the field of modeling or acting.
AREOLAR
#2) This approach involves an incision being made along the areola, which is used to insert the implant. This approach often leaves a noticeable scar around the areola. Since Asians tend to have a small areola, the incision that can be created is usually less than 3cm, making it difficult to insert the implant cleanly without stretching the areolar skin or damaging the implant. Furthermore, if this incision is used twice (i.e., in breast augmentation revision), the nipple can point downward and puckering of the areolar scar may occur.
INFERIOR BREAST CREASE/INFRAMAMMARY FOLD (IMF)
#3) This incision location has the advantage of making the surgery simple. It allows good visualization and can allow bloodless dissection. Bloodless surgery helps decrease capsular contracture from occurring. Furthermore, this incision allows revision surgery to be performed with ease. One disadvantage is it leaves a scar on the breast. Therefore for Asians and African-Americans, this incision requires precise and meticulous wound closure. This approach yields the most consistent aesthetic results.
UMBILLICAL
This approach involves an incision being made in the navel where the implant is inserted, but often results in a scar on the navel which is not easily visible. This approach can only be used with saline implants. Due to the limited incision size, this approach cannot be used for silicone implants. Additionally, this approach can result in asymmetrical breasts, excessive bleeding during surgery, chest and abdominal muscle damage resulting in pain and discomfort following the procedure, and an increased rate of capsular contracture (i.e., hardening of the breast). Furthermore, this approach is ineffective for correcting sagging breasts since specific dual plane technique, which corrects sagging breasts, cannot be performed.
Implant Safety

Throughout this period, many other multi-center and international studies reported on the safety of using silicone implants during breast augmentation. Research and clinical studies found no correlation between silicone implants and autoimmune diseases or cancers. In 2004, Canada re-approved the use of silicone implants and in 2006, the US Food and Drug Administration (FDA) re-approved used of silicone gel implants for cosmetic purposes. This ended the silicone gel implant controversy.
Implant Shells
All breast implants have strong, elastic silicone shells that are either textured or smooth.
TEXTURED
The textured type consists of concave and convex surfaces producing a cobble stone appearance. This surface type was designed to allow the implant to integrate with the breast tissue to minimize capsular contracture. There are reports of textured type implant shells having lower instances of capsular contracture. However, clinical findings are minimal. This type of implant does not need for breast massage and minimal risk of capsular contracture. However, since this implant shell type design is relatively new, there are less known long-term results compared to the smooth. Furthermore, there is less implant mobility compared to the smooth.
SMOOTH
The smooth type of implant, the original breast implant shell design, is smooth in appearance and feel. Results of long-term are known. However, in certain conditions, the implant has been known to move too much. If capsular contracture already occurred in a patient with the smooth type of implant shell, changing the implant to a textured type of shell will not decrease future capsular contracture rate.
Implant Contents
The contents of a breast implant can vary, but some of the more popular options are saline (i.e., salt water), silicone gel, polysaccharide, and vegetable oil.
SALINE

Records of long-term usage exist, and if the implant ruptures, the implant will change shape rapidly and can be easily noticed – allowing the patient to respond. Additionally, if the implant ruptures or leaks, the saline is easily absorbed without harming the body. However, saline implants are not recommended for thin patients because of implant palpability (i.e., easily seen or felt). Furthermore, subtle waves may be seen by the implant when viewed from the side profile, and there is a loss in volume over time.
COHESIVE SILICONE GEL
The content of the implant is silicone gel. The shape can be either round or tear-shaped. Older silicone gels consisted of a more liquid substance, but newer silicone gels are firmer and more cohesive. If the shell of the implant does rupture, the probability of the silicone gel leaking to nearby tissue is extremely low. Furthermore, the silicone gel now stays within the scar tissue that normally forms around the implant; therefore, the silicone generally will not make contact with a person’s breast tissue. The feel of silicone gel implants is softer than saline, and unlike saline implants loss of volume does not occur with time. However, if the implant ruptures, the silicone may migrate outside the implant shell. Additionally, if rupture does occur, it may be possible not to notice a change. Therefore, periodic yearly breast exams are recommended.
Implant Location
The breast implant can be placed in 4 different areas:
- Subglandular, above the pectoralis major muscle
- Subpectoral, under the pectoralis major muscle
- Dual Plane, under the pectoralis major muscle except the most inferior aspect of the breast
- Subfasical, above the pectoralis major muscle but under its fascia.
Subfasical is the most recent implant position placement technique that was originally described in Brazil.
SUBGLANDULAR PLANE IMPLANT LOCATION
This plane is underneath the breast gland but above the pectoralis muscle. This plane is applicable for patients with a decent amount of breast tissue or droopy breast. The advantage of this plane is ease of dissection. The disadvantage is that this dissection plane is associated with a higher rate of capsular contracture. For thin patients or patients with a small amount of breast tissue, the implant can be palpable.
SUBPECTORALIS MUSCLE PLANE IMPLANT LOCATION
The implant is placed below the pectoralis muscle in this plane. Implant palpability is decreased and the capsular contracture rate is lower than subgandular plane implant placement method. But this plane placement is not applicable in droopy breasts or breasts with a short nipple to inferior breast crease distance. In the case of droopy breasts or breasts with a short nipple to inferior breast crease distance, the dual plane method is the treatment of choice.
DUAL PLANE IMPLANT LOCATION
In this approach, most of the implant is placed below the muscle. At the inferior region of the breast, the implant is placed under the breast gland. This particular technique is ideal for droopy breasts or breasts with short nipple to inferior breast crease distance. The dual plane technique is also used to place an implant that is slightly larger than the patient’s breast dimension. By utilizing both planes, the patient’s desired larger breast size can be created.
SUBFASCIA PLANE IMPLANT LOCATION
Subpectoral muscle placement and dual plane method utilize the muscle to cover the implant so that capsular contracture and implant palpability rates are low. However, as the muscle covering the implant contracts, the implant and the breast itself may move. On the other hand, the subfascia method offers the advantage of muscle utilization (decreased implant palpability) without its disadvantages (implant movement). Developed in Brazil in the late 1990s, this method utilizes the thin pectoralis major fascia to cover the implant. Therefore extremely meticulous technique is required to create a space for the implant to be inserted. This is the most recent and advanced breast augmentation surgical technique. This method does not cut pectoralis major muscle to insert the implant. Therefore pain is minimal compared to any other technique that involves utilizing the muscle to cover the implant.
Advantages
- A variety of different Breast Augmentation approaches and implant options
- A body contour that is beautiful, sensual, and proportional
Disadvantages
- Minor swelling
- May involve a relatively lengthy recovery time
- Loss in volume over time
- As with all surgical procedures, there is also some risk of infection
Surgical Duration
The surgical duration will vary based on the approach and implant type used, but the average is 1 to 2 hours.
Anesthesia Options
The choice of anesthesia is given to the patient and the entire procedure may be done under local anesthesia (i.e., a method used by Dr. Kenneth Kim that numbs any sensation on and/or around the surgical site. This is often done through the direct injection of anesthesia at the surgery site and may be accompanied by a mild oral sedative to help ease tension and relax the patient during surgery), intravenous anesthesia (i.e., a method used to render a patient temporarily sedated during surgery), or general anesthesia (i.e., a method used to render a patient temporarily unconscious, paralyzed, and intubated with a breathing tube during surgery).
Recovery Time
The recovery time for this procedure will vary based on the approach and implant type used, but the typical recovery is as follows:
- Return to normal activity in 1 day
- Suture removal in 1 week
- Reduced swelling in 3 weeks to 1 month
When surgery is performed properly, the person should experience minimal post-operative pain, discomfort, and swelling.
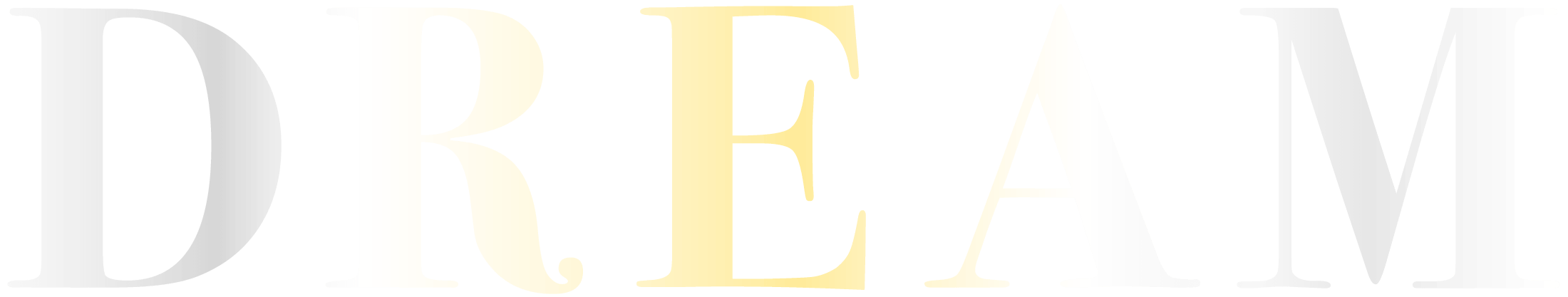
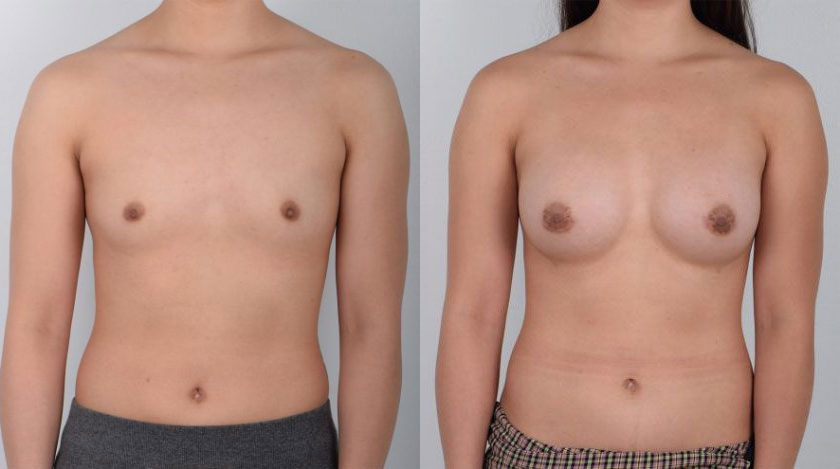
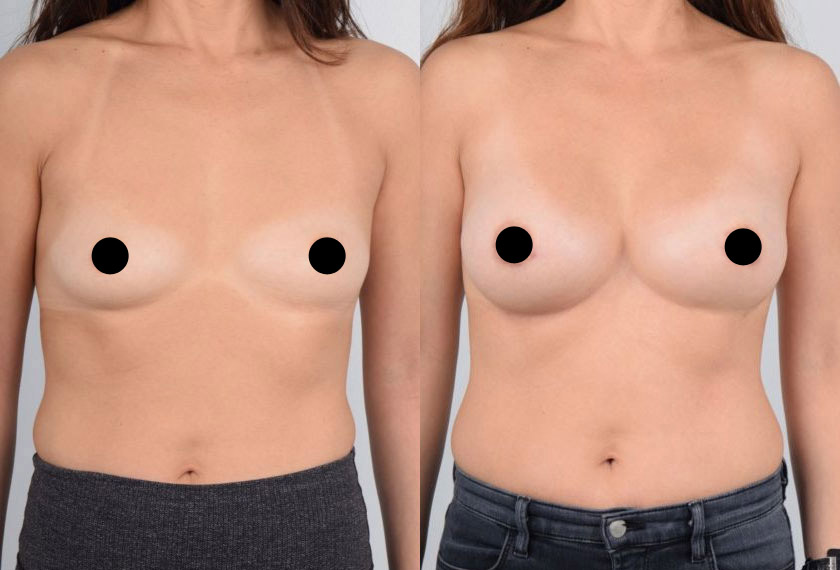
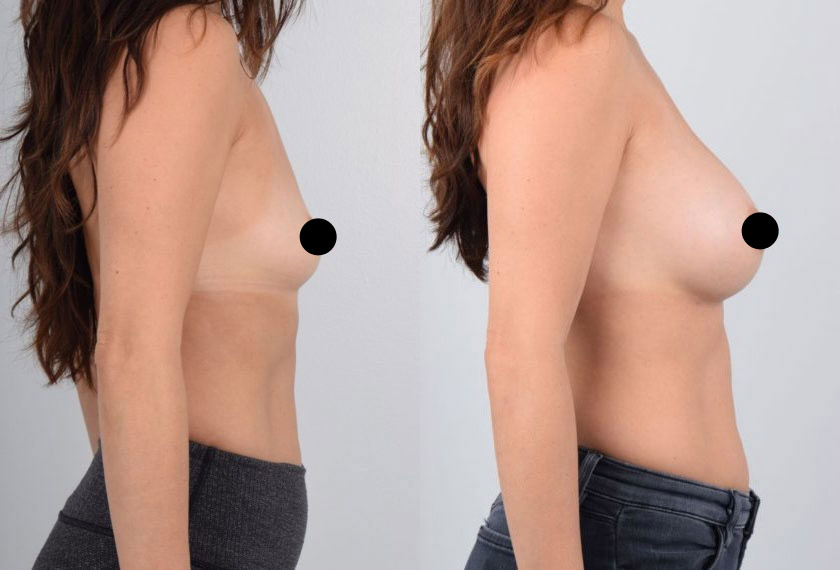
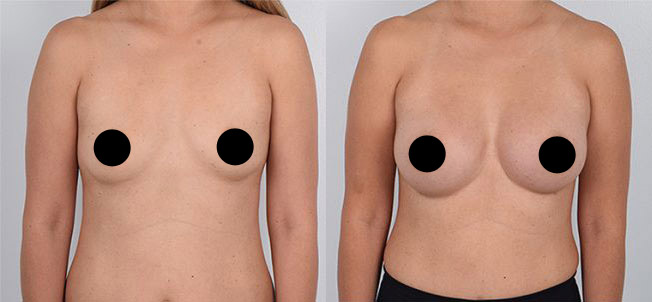
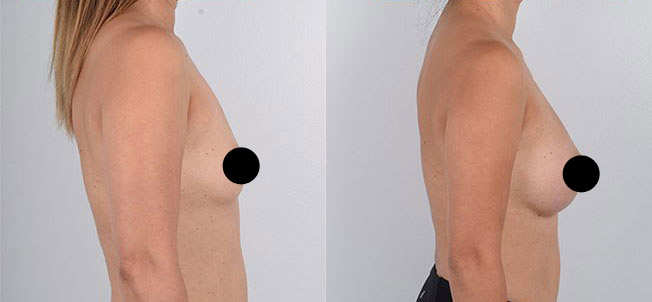
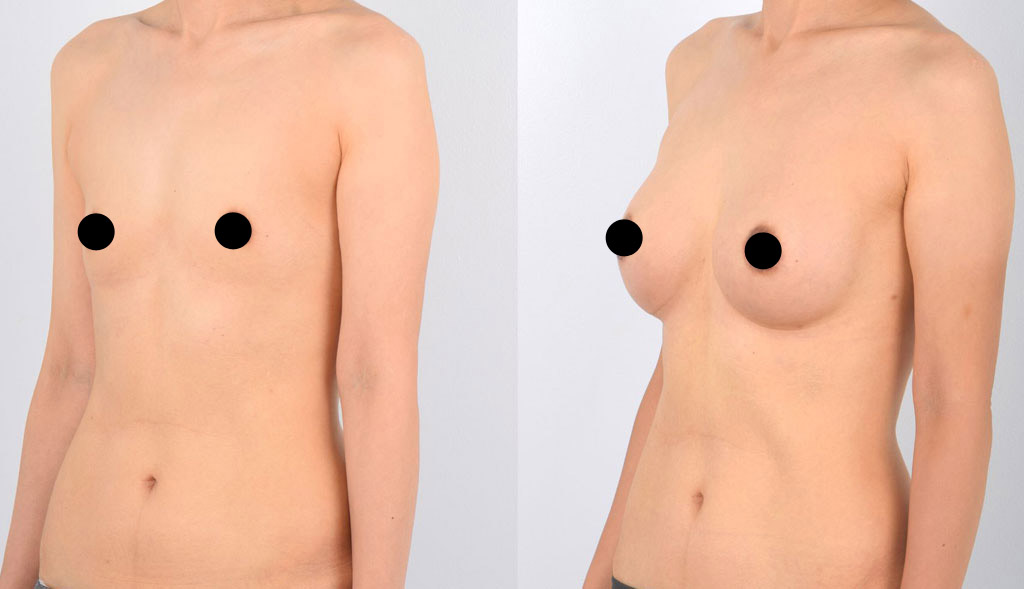
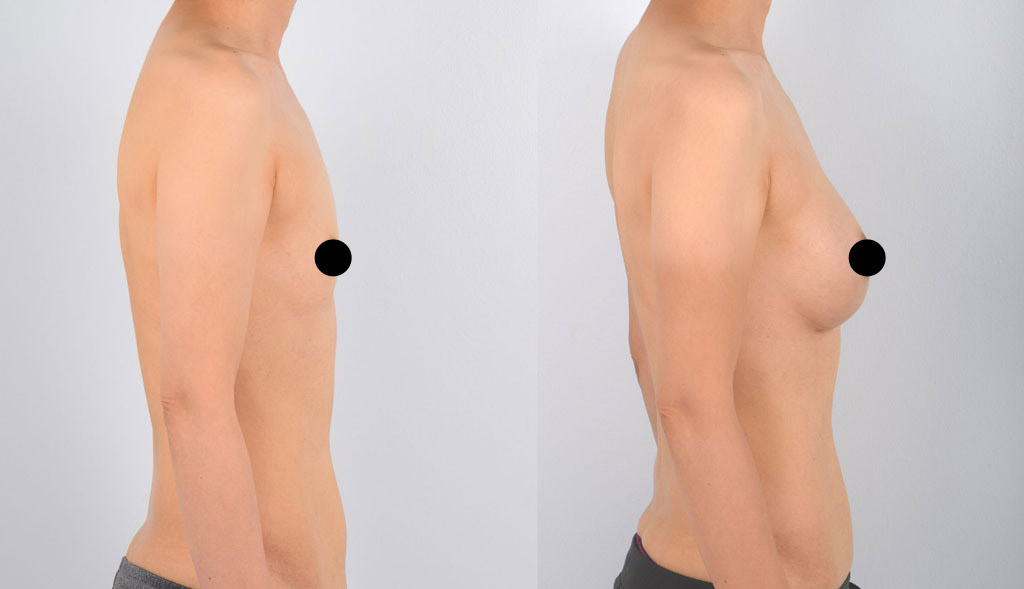
Expected Results
- A beautifully contoured, proportional, and symmetrical breasts
- A more attractive body shape
- An overall more aesthetically pleasing look
Medical Publications
The Use of a Retromammary Adipofascial Flap in Breast Augmentation for Patients with Thin Soft Tissue
Aesth Plast Surg
21 May 2018 / Accepted: 14 August 2018
The application of a retromammary adipofascial flap is an effective method of producing natural breast shape and providing additional soft tissue to the caudal breast region.

Plastic and Reconstructive Surgery, Vol. 135, No. 3
March 2015
The transareolar-perinipple (areolar omega) zigzag incision resulted in satisfactory postoperative scarring and surgical results in Asian patients. This method increases the opening of the areolar incision and can be performed in patients with small (<3.5 cm) areolas. This approach can be an alternative in patients who are prone to hypertrophic scarring.