Facial Bone Surgery

Introduction

Cheekbone Reduction (Zygoma / Malar Reduction)
The Advantages of Dr. Kim's Approach
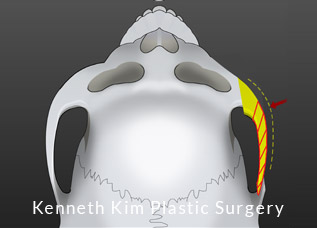
1. Osteotomy (Cutting of the bone)


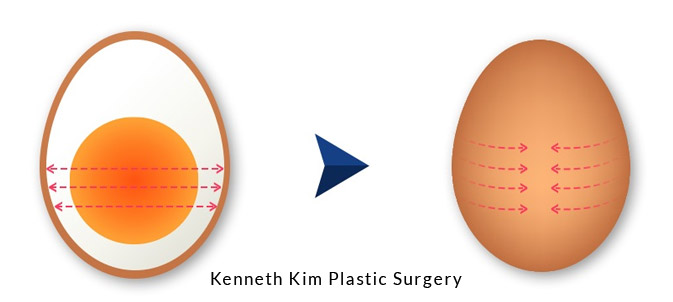
2. Bone Stabilization

3. Soft Tissue Elevation / Support


V-Shaped Jaw Reduction Surgery
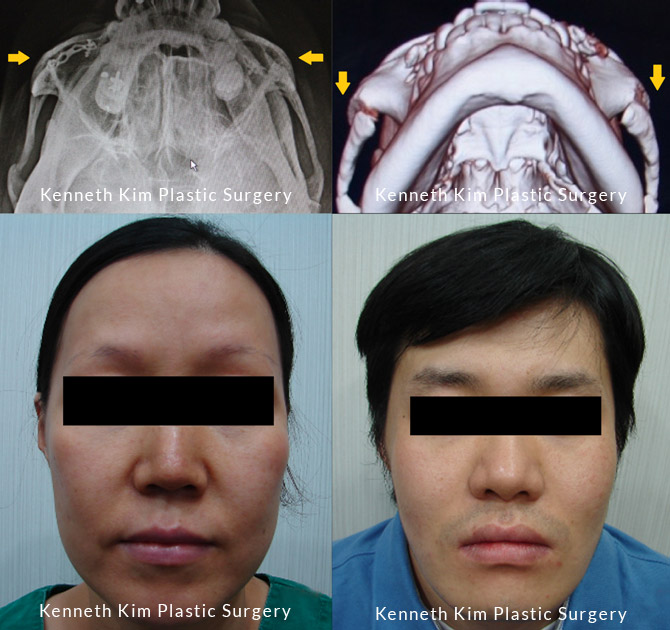
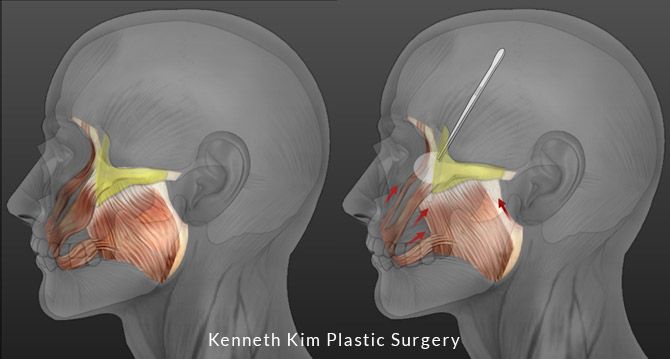
This surgery involves removal of the flaring/protruding angle of the mandible (jaw bone). Jaw reduction surgery in particular can be a high-risk bone surgery. One reason is the negative sequela which is postoperative soft tissue drooping. The other is more serious which is significant bleeding or even life-threatening bleeding.
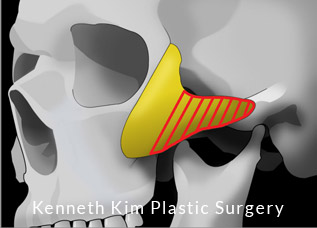
There are vessels, specifically the retromandibular blood vessel, that is situated at the back/posterior to the mandibular angle. When approaching this area from the mouth (intraoral), the surgeon cannot see the vessel. Therefore, during cutting, the saw instrumentation can cut the vessel or during the bone detachment after the cut, the vessel can rupture because it has not been fully mobilized from the bone. The inadequate vessel mobilization occurs because the vessel cannot be seen and the angle of the intraoral approach makes it difficult to detach the vessels. Both possible scenarios (saw cutting the vessel or tearing of the vessel during bone removal) can cause significant bleeding that is difficult to stop due to the lack of exposure and visibility. The only way to stop this type of bleeding is to pack it and let it stop over multiple hours of bleeding as it cannot be cauterized. This can lead to significant blood loss requiring a large amount of blood transfusion and can even be fatal. These complications still occur annually since its inception in South Korea and the rest of Asia where jaw reduction surgery is most often performed. Among the plastic surgeons in South Korea, a small percentage perform mandible surgery due to the risks and complications.
Dr. Kim believes that all elective surgeries should be safe and performed without taking these types of risks.
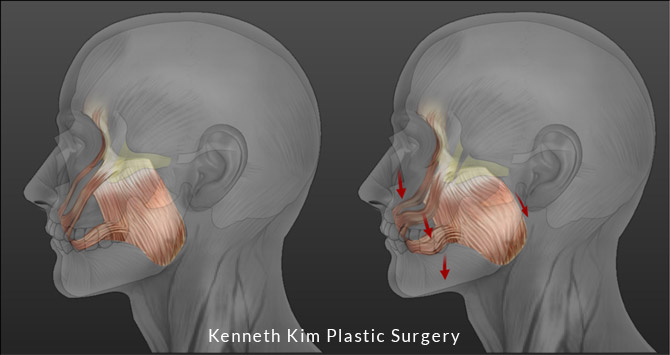
His surgical technique is designed to avoid these complications. He accomplishes this by having direct visualization of the vessels and surgical region and fully mobilizing the soft tissues and vessels away from the bone that is to be cut. After cutting and removal of the bone, the mobilized soft tissue and vessels are undisturbed. Hypothetically, if there is bleeding, because Dr. Kim has a direct view of the vessels, the bleeding can be stopped. Furthermore, the advanced instrumentation he uses also ensures that nothing but the bone is cut by the saw. What this means is the state-of-the-art technology will not cut soft tissue or vessels, thus ensuring another margin of safety.
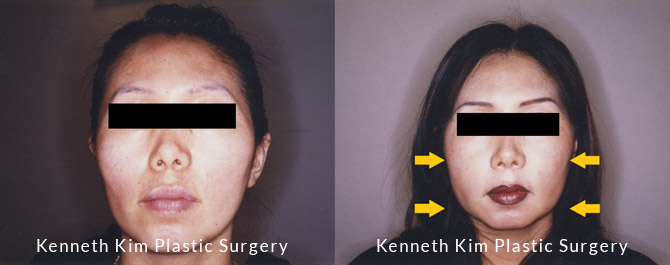
The traditional approach to jaw reduction involves operating through the mouth and detaching the soft tissue from the bone. When the reduction occurs, the soft tissue remains detached and therefore starts sagging following surgery. Once the soft tissue has been detached, the aging process accelerates postoperatively. Over time, the patient will appear older than their age group and essentially lose the effect of the jaw reduction because the detached soft tissue will descend, creating a rounder, fuller jawline, going against the desired V-shape. Dr. Kim’s approach to jaw reduction surgery entails not only reducing the flaring jaw bone but also repositioning the soft tissue so there is no soft tissue descent or drooping and the patient maintains a V-shaped face.

Genioplasty (Chin Augmentation)
Consultation
Choosing an Expert
Bone surgery requires precision, an aesthetic eye, and a thorough understanding of bone biology and biomechanics. Dr. Kim performs the most advanced surgical techniques that he has received extensive training on and has further developed throughout his career. He understands bone regeneration and healing at the molecular and cellular levels.
As a Howard Hughes Medical Institute fellow, Dr. Kim conducted research on growth factors such as bone morphogenetic proteins (BMP) and transforming growth factor beta (TGF-β) and published numerous peer-reviewed scientific publications on the subject of bone healing at the molecular and cellular levels. In addition, Dr. Kim has worked with the top biomechanical engineers in Switzerland as an AO Research and Development fellow, the first U.S. resident to be inducted as a fellow at the AO headquarters in Switzerland. During his fellowship, he designed and developed instrumentation and surgical processes for facial bone reconstruction utilizing minimally invasive methods. He worked with the leading craniomaxillofacial reconstructive surgeons in Europe, North America, and Asia. He was also an instructor at the AO Institute, teaching surgeons the fundamentals of facial reconstruction. Furthermore, he received advanced training as a facial trauma and reconstruction fellow at UC Davis Medical Center where he acquired the skill set to perform complex bone reconstruction. He conducted research and pioneered utilization of real-time 3D CT image guided surgery on facial bone to improve surgical precision. He also designed the method to build customized implants for craniofacial defects with ultra-high resolution 3D renderings.
Furthermore, he has trained and collaborated with numerous pioneers of bone surgery in South Korea, where bone surgery originated and where innovation occurs most. Dr. Kim serves as a clinical instructor at Seoul National University and is conducting research on innovative approaches to bone contouring, detailed anatomy of facial nerves and vessels, and improved safety in bone surgery.

Dr. Kim’s Principles to Facial Bone Surgery:
Facial Aesthetics: A surgeon must have a keen sense of aesthetics and be able to operate on all aspects of the face and body. The facial skeleton is in proportion to the frame of the body and our distinguishing features (eyes, nose, and lips) sit on the dimensions of the facial skeleton. A surgeon must be able to distinguish whether to contour the facial bone or to improve the appearance of other features such as the eyes, nose, lips, and facial fat and muscles to achieve desired and optimal results. A plastic surgeon must be able to operate on all aspects of the face and body to create balanced proportions and the most beautiful face for the patient.
Biomechanics: Facial bone exists not only for aesthetics but also as a foundational pillar for the soft tissue and as protection for the brain and vital structures of the face. Therefore, facial contouring surgery which involves cutting the facial bone and reconstructing it must be done in a biomechanically stable form. A plastic surgeon must have extensive knowledge on biomechanical engineering in order to reconstruct the facial skeleton in the most stable manner.
Soft Tissue: Bone surgery without addressing soft tissue is an incomplete surgery. In order to have access to bone for any type of bony manipulation requires degloving or detachment of the surrounding soft tissues (i.e. muscles, fat, vessels, and nerves). Traditional facial bone surgery has been focused on only bone manipulation. Thus, the negative sequela of bone surgery have been early aging due to drooping of the soft tissue. A plastic surgeon must address soft tissue re-elevation in order to have a complete result, where the patient’s face becomes more aesthetically pleasing and more youthful.
Bone healing: Contrary to popular belief, bone is not a static structural entity. The bone is made up of living cells and undergoes constant remodeling which means it goes through growth and degeneration. A facial bone surgeon must have a deep and thorough understanding of the physiology of bone cells and its growth to ensure that they maintain their natural progression of cellular life cycle after bone cutting and reconstruction. In standard bone cutting, tremendous heat is produced during cutting which can burn and kill the living bone cells. A surgeon must use state-of-the-art technology where bone cutting does not deliver additional heat so the bone cells are not negatively affected. In addition, a surgeon must understand how growth factors that the bones release are altered during the healing process and must optimize the bone physiology for rapid and stable bone healing.
Safety: Bone contouring surgery just like any other plastic surgery is an elective procedure. Therefore, a patient should not take chances with safety. Surgical risks include (1) anesthetic risks and (2) surgical complications that arise from the technical aspect of surgery. Dr. Kim places the utmost emphasis on patient safety and designs his surgery from beginning to end with patient safety in mind, so the patient does not need to experience unnecessary risks and complications. Dr. Kim accomplishes this by using local anesthetic, thus avoiding the need for general anesthesia or IV sedation, and by practicing ultra-precision surgery leading to minimal bleeding, thus providing for clear visualization. With safety in mind, facial bone contouring surgery can be performed with ease and comfort for the patient and provide rapid recovery.
Medical Publications
 A Comprehensive Assessment of Soft-tissue Sagging
after Zygoma Reduction Surgery through Artificial
Intelligence Analysis
A Comprehensive Assessment of Soft-tissue Sagging
after Zygoma Reduction Surgery through Artificial
Intelligence Analysis
Received for publication March 4, 2024; accepted June 21, 2024
Background: Overdevelopment of zygomatic bones often results in protrusion and flaring of the midfacial region. This makes the face appear squarer than the more favorable oval shape. Therefore, zygoma reduction surgery has become a commonly performed procedure in patients seeking to obtain an ideal facial shape. Facial soft-tissue ptosis is one of the main complications of zygoma reduction surgery. Previously, the evaluation of cheek soft-tissue ptosis was subjectively based on patients and surgeons. Our study aimed to provide an objective evaluation of softtissue sagging in the cheek region after zygoma reduction surgery using artificial intelligence (AI).
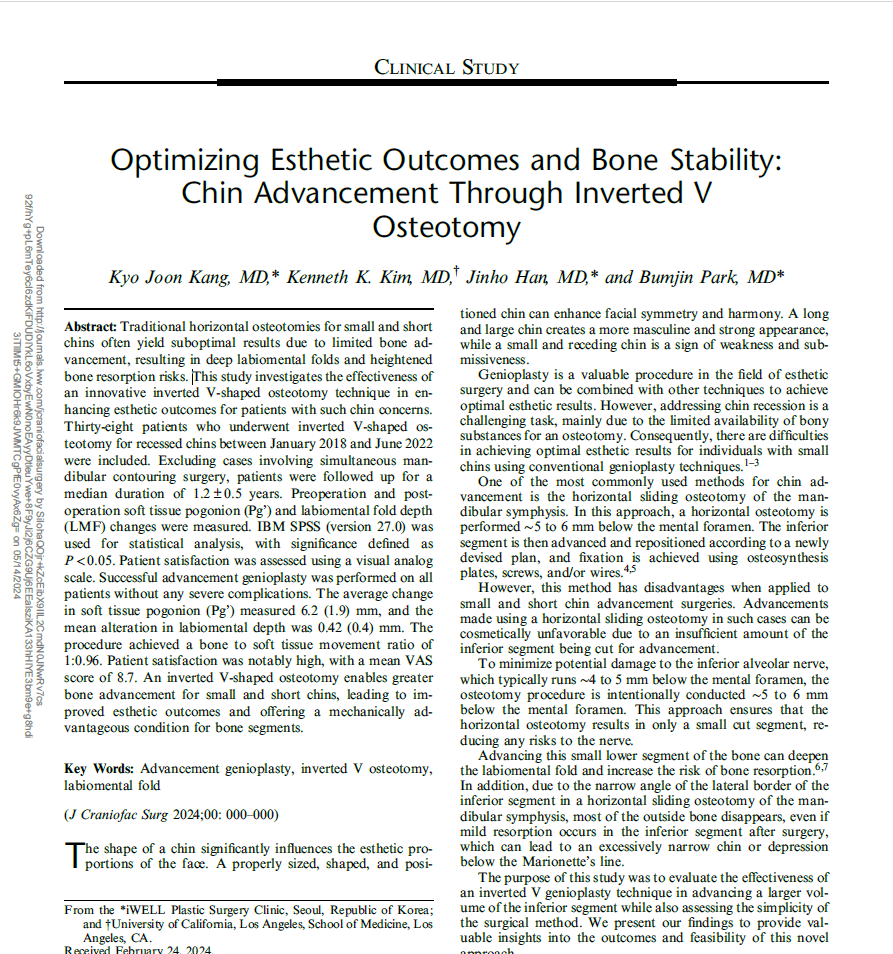 Optimizing Esthetic Outcomes and Bone Stability:
Chin Advancement Through Inverted V
Osteotomy
Optimizing Esthetic Outcomes and Bone Stability:
Chin Advancement Through Inverted V
Osteotomy
Received February 24, 2024. Accepted for publication April 3, 2024.
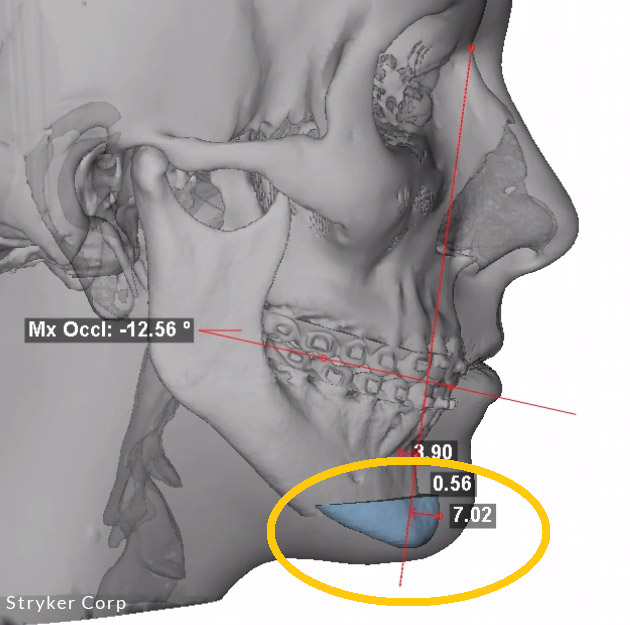
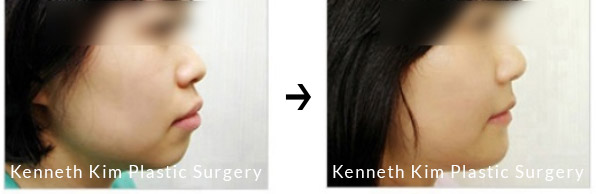
Abstract: Traditional horizontal osteotomies for small and short chins often yield suboptimal results due to limited bone advancement, resulting in deep labiomental folds and heightened bone resorption risks.
 The Rationale of Coronal Approach to Malar/Zygoma Reduction
The Rationale of Coronal Approach to Malar/Zygoma Reduction
Received for publication July 24, 2023; accepted August 16, 2023.
Background: Malar/zygoma reduction is an effective procedure to change a broader, flatter facial appearance to an oval facial shape. Of the intraoral and coronal approaches, the intraoral is the more commonly used technique than the coronal, due to the perception that complications with the coronal approach are significant, and intraoral results are satisfactory. We compared the postoperative effects of both approaches.